Since we opened in 2004, the extent of our reach and scope has surpassed even our own expectations. 2023 has been particularly transformative, demonstrating our capacity to further expand our impact. Let’s take a moment to revisit the standout moments and accomplishments that have shaped our year at CSDS.
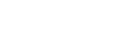
We delivered training in record numbers
We delivered 46 courses over 524 sessions, engaging a total of 3,121 participants. Our most popular course was Advanced Life Support having run over 143 sessions across Brisbane, Roma, Charleville, Bowen, Cairns, Norfolk Island, Cooktown, Weipa, and Thursday Island.
We expanded our course catalogue
We launched 12 new online courses and various updates across our online course catalogue. Some highlights include Electrocardiograph rhythm interpretation, Defibrillation and other uses for a defibrillator, Monitoring equipment, Intravenous iron: Administration and management, Intravenous Iron: Prescribing, Trauma – Acute compartment syndrome, and Water immersion for labour and birth.
We also launched our Water Immersion for Labour and Birth course, developed in response to a year-long training needs analysis highlighting policy inconsistencies and a significant gap in standardised education on water immersion during labour. The online course component has attracted 751 enrolments, with 512 participants completing it. Furthermore, 89% of participants (n=450) responded to our feedback survey, giving the course an overall rating of 4.68 out of 5 stars.
Our impact on our network continued to grow

We supported over 130 Pocket Centres throughout the state, enabling them to conduct 5,300 simulation events. This support contributed to an impressive total of over 130,000 educational hours, using 2,200 different pieces of equipment. Beyond this, we dedicated over 6,300 hours to the maintenance, repair, and support of simulation equipment and successfully dispatched over 2,215 packages to assist these Pocket Centres.
We have provided translational simulation events before the opening of the Metro North Satellite Hospitals at Caboolture and Kallangur. These events were crucial in identifying and resolving potential safety issues, ensuring that, from the very first day, patients receive the safest and most effective care possible.
Additionally, we supported the Bundaberg Hospital, Logan Hospital Expansion Project, and Rockhampton Hospital by providing crucial facility upgrades. Our efforts focused on delivering the necessary audio-visual technology support, enabling our simulation educators to efficiently and effectively create clinical simulation environments. This assistance is part of our ongoing commitment to enhance healthcare training infrastructure across various institutions.
We went rural and remote

The significant growth in demand for Maternity Education this year prompted us to expand courses and rebrand the Maternity Education Program to Queensland Maternity Education (QME), aligning with our broader outreach across the state. We expanded our licencing agreements to Torres and Cape, Townsville, Mackay, Central Queensland, South West, Darling Downs, and Metro South.
In addition, we gained approval of recurrent funding for us to deliver our accredited maternity education programs across the state under a $2.2 million Rural and Regional Birthing Services Grant. This funding will allow us to deliver standardised, ongoing training for up to 400 staff every year for the foreseeable future.

Queensland Trauma Education‘s highly successful course QTEC continues its successful run at CSDS, but has also expanded to regional, rural, and remote centres. We continue to receive strong interest with a waiting list of attendees eager to secure their places. QTEC was recently licenced by the Townsville HHS, enabling easier access for clinicians in the Far North.
Since the launch of this program, 205 clinicians (from nursing, midwifery, medical, and allied health fields) have attended one of 18 face-to-face courses, or 8 on-the-road and train-the-trainer courses. There have been 64,000 website visits, over 11,000 active users (across 10 countries), and over 9,000 downloads of training resource kits. 100% of responders also strongly agreed or agreed that the knowledge and skills gained would result in improved clinical practice. These data suggest that the innovative approach of QTE meets the identified needs to improve trauma care education and patient care.
We engrained research and innovation

We have collaborated with Telehealth, Griffith University, and Jamieson Trauma Institute on a project focused on exploring the feasibility of using augmented reality headsets to guide remote healthcare workers. This innovative approach is part of our broader commitment to integrating technology in healthcare.
Building on this theme of innovation, our hosted students have made significant strides this year. In July, Dr Jasmine Antoine successfully passed her confirmation milestone and secured a $150,000 Betty McGrath Education Seeding Grant for her project “Enhancing Trainee’s Technical and Non-Technical Skills in Neonatal Intubation”. Additionally, we hosted two Masters of Organisational Psychology students, Rebecca Wang and Joseph Tully. Rebecca developed a heuristic guideline for clinical emergency algorithms, while Joseph focused on enhancing the workflow and efficiencies of our course delivery.
In the realm of research, our efforts have been widely recognised. Four manuscripts have been accepted into the Australian Nursing and Midwifery Journal, covering diverse topics from maternity emergency programs and water immersion in labour and birth, to the use of 3D animation in midwifery education. This recognition is a testament to our team’s dedication to advancing healthcare education and practice.
Further highlighting our expertise, Dr Kirsty McLeod presented “A Nursing Tool to Improve the Flow and Safety of Patients Receiving a Lumbar Puncture” at the International Forum on Quality and Safety in Healthcare in Melbourne. Kirsty’s work didn’t stop there; she was also the lead investigator on a Metro North SWIFT Grant, winning $14,902 for a project aimed at “Implementing a Lumbar Puncture Nursing Assessment Tool to Support Clinical Practice and Improve Patient Care”. Her participation as one of only three presenters at the Emerging Researchers and Practitioners in Human Factors in Healthcare webinar further underscores our organisation’s influence in the international healthcare community.
Complementing these achievements, Dr Mia McLanders has been at the forefront of engraining research into our mission. As a Chief Investigator, she played a pivotal role in winning a $2.8M MRFF grant for “Genetic Testing for Polygenic Risk: Developing Education Resources for Healthcare Professionals and Risk Communication Aids for Patients”. Her leadership in securing a $25,000 Metro North SWIFT Grant for “Securing Endotracheal Tubes Safely and Accurately in Tiny Patients” and co-authoring an award-winning abstract at the Australasian Neurosciences Nurse Association Conference for “The development and Implementation of the Adult Neurological Early Warning Tool” further demonstrates our commitment to advancing healthcare through research into practice.
Our partnerships made a difference
Earlier this year, we collaborated with the Metro North Clinical Governance and the Clinical Leadership Excellence Queensland to develop the Safety and Quality Education Program (SQEP); a direct response to the Metro North Hospital and Health Services’ Caboolture Hospital Independent Governance Review. This project addressed critical patient safety and quality gaps through comprehensive and multimodal educational resources. We launched all these resources on our Safety and Quality Education program website.
SQEP has been widely praised for its comprehensive range of resources. SQEP’s website has attracted 30,000+ page views while our online courses have garnered over 14,000 responses and achieved an average rating of 4.7 out of 5. Our partnership with Clinical Leadership Excellence resulted in 90+ virtual educational sessions that have trained 600+ staff members.
We also collaborated with the Queensland Spinal Cord Injuries Service to produce an online knowledge hub for healthcare professionals and patients dealing with spinal cord injuries across Queensland and Northern NSW. This project addressed the lack of proficiency among many healthcare professionals in managing spinal cord injuries due to the condition’s rarity, bridged the gap in specialist care access, and empowered non-spinal cord injury specialist healthcare providers in remote and regional areas.

We also partnered with St. Rita’s College and Bray Park State High School to exemplify the importance of experiential learning in fostering a deeper understanding of scientific principles. These visits were an immersive experience and offered an opportunity to bridge theoretical knowledge with real-world applications through hands-on activities and skill stations.
Our partnerships extended beyond Queensland. Together with the Northern Tasmanian Health Service, we collaborated with them to incorporate our Introduction to Peripheral Intravenous Cannulation (IPIC) course into Tasmania’s cannulation program. This partnership marks a significant step in enriching the resources available to healthcare professionals in Tasmania, addressing the challenges of limited resources in smaller states.
We were recognised

On December 15th, Metro North Health honoured the remarkable achievements and commitment of its staff. This year saw an impressive 180 nominations spanning ten categories. We proudly stood as finalists in four categories, including Leadership, Excellence in Performance, People Focus, and Innovation.
Ultimately, our very own Kate Britton was honoured with this year’s Leadership Award. Kate’s outstanding leadership qualities, marked by her steadfast commitment to collaboration, trust, and recognition, have played a pivotal role in securing various significant funding grants. In addition to Kate’s remarkable achievement, we would also like to celebrate the success of three of our projects that were finalists on the night:
- Excellence in Performance: Safety and Quality Education Program, in partnership with the Metro North Clinical Governance and Clinical Leadership Excellence Queensland.
- Innovation: Focal Neurological Observation Tool, an initiative in partnership between RBWH and Dr Mia McLanders.
- People Focus: Online Knowledge Hub for Spinal Cord Injury Care, an inter-HHS project with the Queensland Spinal Cord Injuries Service.
As the holiday season draws near, our team is preparing to take a well-deserved break, returning refreshed and recharged on the 8th of January. With warm regards from all of us at CSDS, we extend heartfelt wishes for a joyful holiday season and a fantastic start to the new year!