Kirsty McLeod, Luke Wainwright and Clinton Henderson from the CSDS collaborated with the Herston Biofabrication Institute, The University of Queensland’s School of Medicine and School of Nursing, and the Intensive Care Services at the Royal Brisbane and Women’s Hospital to explore the challenges associated with proning patients (i.e., turning face down) in the ICU. The outcomes and recommendations from this work were recently published in “Human Factors and Ergonomics in Manufacturing and Service Industries” in a paper titled “Applying a human factors approach to proning pillows in the ICU: Opportunities for redesign”. The outcomes from this research provide a guide for the improved design of proning pillows to reduce the risk and prevalence of pressure injuries commonly experienced by patients in the ICU.
Abstract
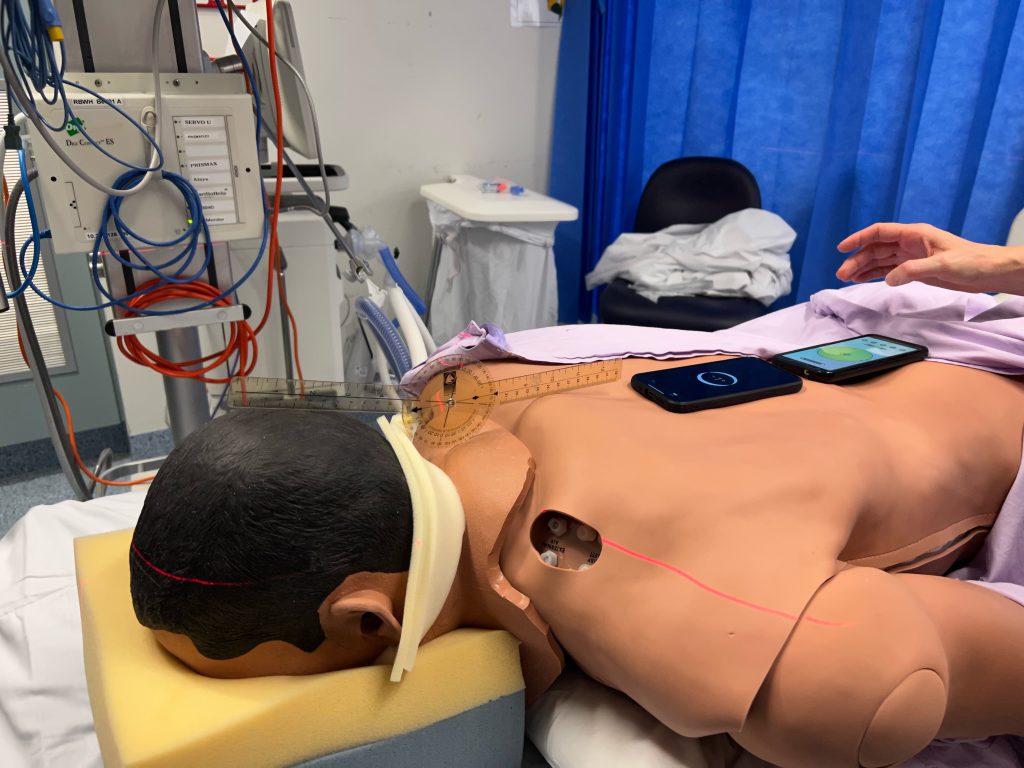
Proning, or turning a patient face down, is a technique used to manage patients with acute respiratory distress in intensive care units (ICUs). Research suggests that the type of pillow used in proning may have a significant impact on patient outcomes and increase the risk of disfiguring pressure injuries to the face. However, there is little evidence surrounding the usability of these pillows in the ICU. The aim of this study was to identify redesign opportunities by understanding how the tools, tasks, people, environment, and organization all interact during proning in the ICU.
Thirty-six ICU clinicians from two Australian public metropolitan hospitals completed an online questionnaire regarding their opinions and experiences with proned patients and the prevention of pressure injuries. Seven ICU clinicians then completed journey mapping activities to document the key workflows, critical incidents, considerations, and personnel involved in managing proned patients in the ICU. Several barriers and facilitators to pressure injury prevention were identified, including interactions between the various tools (e.g., proning pillows with one opening limits the management of several medical devices), the tasks (e.g., high frequency of repositioning), the people (e.g., clinical inexperience, patient features), the environment (e.g., limited availability of tools), and the organization (e.g., limited number of staff to support tasks).
This holistic approach revealed several opportunities for the redesign of proning pillows and associated systems. Key takeaways include the limitations of a one‐size‐fits‐all approach to proning in the ICU context, and the need for flexibility and customization to improve proning pillows, associated medical devices, prophylactic dressings, aids, and processes.
Do you have ideas or requests for improving healthcare through training, collaboration and innovation? Reach out to the CSDS team via the CSDS Idea and Request Form.